Connect With Us
Blog
Items filtered by date: April 2022
Standing for Long Periods of Time May Cause a Heel Spur
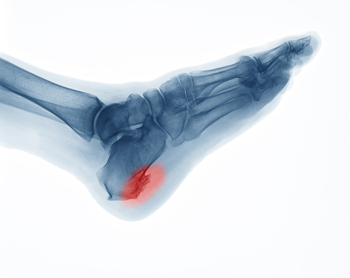
Research has shown that for every mile walked, there are sixty tons of stress that goes through the foot. Heel pain can indicate a heel spur may have developed and can become worse without proper treatment. It is defined as a bony growth that forms at the base of the heel and can cause severe pain and discomfort. This condition can come from standing on your feet for most of the day, or from wearing shoes that do not fit correctly. Some patients find it helpful to practice specific stretching exercises, and this may help them to find mild relief. Additionally, when proper stretches are performed, it may give the foot the ability to have increased range of motion and flexibility. Obese patients may find it beneficial to lose extra pounds and wearing heel pads may provide temporary relief from the heel spur. If you have developed this ailment, it is suggested that you are under the care of a podiatrist who can properly treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from Omega Podiatry. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Los Angeles, Huntington Park, and Reseda, CA . We offer the latest in diagnostic and treatment technology to meet your needs.
Gout Pain Can Be Managed
Foot Conditions May Develop From Wearing Flip Flops
 The idea of wearing flip flops is appealing to many people. They are easy to wear and are available in a variety of styles and colors. However, research has indicated that this style of shoe may cause damage to the feet. A person's gait or walking pattern could be negatively impacted in order to accommodate for the lack of arch support and cushioning, and the ankles may turn inward. It can also be easier to stub your toe while wearing flip flops, which may result in a broken toe. Additionally, the toes are constantly gripping the front of the shoe to keep it securely on the foot. This repeated action may cause strain in the overall foot, or cramps may develop as well. There are several other foot conditions that can result from wearing flip flops as well. If you are interested in learning more about the effects flip flops can have on the feet, please speak with a podiatrist.
The idea of wearing flip flops is appealing to many people. They are easy to wear and are available in a variety of styles and colors. However, research has indicated that this style of shoe may cause damage to the feet. A person's gait or walking pattern could be negatively impacted in order to accommodate for the lack of arch support and cushioning, and the ankles may turn inward. It can also be easier to stub your toe while wearing flip flops, which may result in a broken toe. Additionally, the toes are constantly gripping the front of the shoe to keep it securely on the foot. This repeated action may cause strain in the overall foot, or cramps may develop as well. There are several other foot conditions that can result from wearing flip flops as well. If you are interested in learning more about the effects flip flops can have on the feet, please speak with a podiatrist.
Flip-flops can cause a lot of problems for your feet. If you have any concerns about your feet or ankles, contact one of our podiatrists from Omega Podiatry. Our doctors will assist you with all of your foot and ankle needs.
Flip-Flops and Feet
Flip-flops have managed to become a summer essential for a lot of people. While the shoes may be stylish and easy to slip on and off, they can be dangerous to those who wear them too often. These shoes might protect you from fungal infections such as athlete’s foot, but they can also give you foot pain and sprained ankles if you trip while wearing them.
When Are They Okay to Wear?
Flip-flops should only be worn for very short periods of time. They can help protect your feet in places that are crawling with fungi, such as gym locker rooms. Athlete’s foot and plantar warts are two common fungi that flip-flops may help protect your feet against.
Why Are They Bad for My Feet?
These shoes do not offer any arch support, so they are not ideal for everyday use. They also do not provide shock absorption or heel cushioning which can be problematic for your feet. Additionally, you may suffer from glass cuts, puncture wounds, and stubbed toes since they offer little protection for your feet.
More Reasons Why They Are Bad for Your Feet
- They Slow You Down
- May Cause Blisters and Calluses
- Expose Your Feet to Bacteria
If you have any questions, please feel free to contact our offices located in Los Angeles, Huntington Park, and Reseda, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Measure for Shoe Size
Always measure your feet if you have any questions about your proper shoe size. You can measure your own feet with a tape measure or ruler, paper, a writing implement, and a chair to sit on while measuring your feet. First, tape the paper to the floor so it will not move. Second, sit on the chair and put one foot on the paper. Make sure to wear socks or foot coverings that you plan to wear with shoes before placing them on the paper. Third, outline the outside of your foot with your pen or pencil. Do this for both feet to check subtle differences that might be present between your feet. Fourth, measure from the tip of the heel to the longest toe of your foot and make a note of the numbers. Finally, do some simple math – subtract 3/16 from the measurement you wrote down to account for the difference between your foot and the shoe. The result is your shoe size! If you have trouble measuring your feet properly or find that you are still not able to find comfortably fitting shoes, see a podiatrist for help in measurements, and shoe suggestions, or to help you detect any other problems that might be going on with your feet.
Getting the right shoe size is an important part of proper foot health. Seek the assistance of one of our podiatrists from Omega Podiatry. Our doctors will provide the care you need to keep you pain-free and on your feet.
Getting the Right Shoe Size
There are many people who wear shoes that are the incorrect size, negatively affecting their feet and posture. Selecting the right shoes is not a difficult process, so long as you keep several things in mind when it comes to choosing the right pair.
- When visiting the shoe store, use the tools available to measure your foot.
- Be sure there is ‘wiggle room’. There should be about an inch between your toes and the tip of your shoes.
- Do not always assume you are the same size, as manufacturers run differently.
- Purchase shoes later in the day, as your feet swell as the day progresses.
- If a shoe is not comfortable, it is not suitable. Most shoes can’t be ‘broken in’, and comfort should be the ultimate goal when it comes to choosing the right pair of shoes
As our feet hold our body weight and keep us moving, it is important to treat them right. Picking the right pair of shoes can provide your feet comfort and mobility without pain.
If you have any questions, please feel free to contact our offices located in Los Angeles, Huntington Park, and Reseda, CA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Best Care For Elderly Feet
 Since it's said that 75% of seniors experience foot problems as they age, it stands to reason that foot care is an important part of their overall health care. If seniors maintain the health of their feet, they will be able to stay active longer, keep better balance and prevent falls (a key reason for injury and hospitalization in elderly years), and remain aware of signs that other health issues might be present (such as diabetes, arthritis and other serious conditions). The elderly should check their feet each day to make sure there is nothing visible that appears unusual (like blisters, swelling, or infections), wash and dry feet daily, trim toenails regularly, tend to any corn or callus, moisturize the tops and bottoms of feet if the skin is dry or cracked, wear well-fitting shoes and socks, and make sure socks are clean and do not restrict circulation or irritate the feet in any way. Regular exercise, eating healthy, and stopping smoking may also contribute to foot health. If a senior is unable to tend to their feet by themselves, it is advisable to set up routine visits with a podiatrist to maintain proper foot care and diagnose and treat any problems as they arise.
Since it's said that 75% of seniors experience foot problems as they age, it stands to reason that foot care is an important part of their overall health care. If seniors maintain the health of their feet, they will be able to stay active longer, keep better balance and prevent falls (a key reason for injury and hospitalization in elderly years), and remain aware of signs that other health issues might be present (such as diabetes, arthritis and other serious conditions). The elderly should check their feet each day to make sure there is nothing visible that appears unusual (like blisters, swelling, or infections), wash and dry feet daily, trim toenails regularly, tend to any corn or callus, moisturize the tops and bottoms of feet if the skin is dry or cracked, wear well-fitting shoes and socks, and make sure socks are clean and do not restrict circulation or irritate the feet in any way. Regular exercise, eating healthy, and stopping smoking may also contribute to foot health. If a senior is unable to tend to their feet by themselves, it is advisable to set up routine visits with a podiatrist to maintain proper foot care and diagnose and treat any problems as they arise.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Omega Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our offices located in Los Angeles, Huntington Park, and Reseda, CA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021